Centralize
All Contracts in a Single, Unified Platform
Predict
Financial Outcomes with Confidence
Measure
Performance Across Contracts in Real-Time
Adjudicate
Monthly and Final Contract Results Effortlessly
Let Us Do the Heavy Lifting in Your Value-Based Care Contracts
Powered by advanced actuarial science, the Arbital platform can handle all of your risk contracts, no matter the complexity.
Automated, Streamlined, Scalable
Turn months of manual work into minutes
Cloud-Based SaaS Environment
Reliable and secure digital infrastructure for all your data needs
Trusted Data Quality
Ensure data integrity with seamless ingestion and swift issue detection
Actuarially-Validated Insights
Access expert analysis against market benchmarks to drive decision-making
Discover the Features
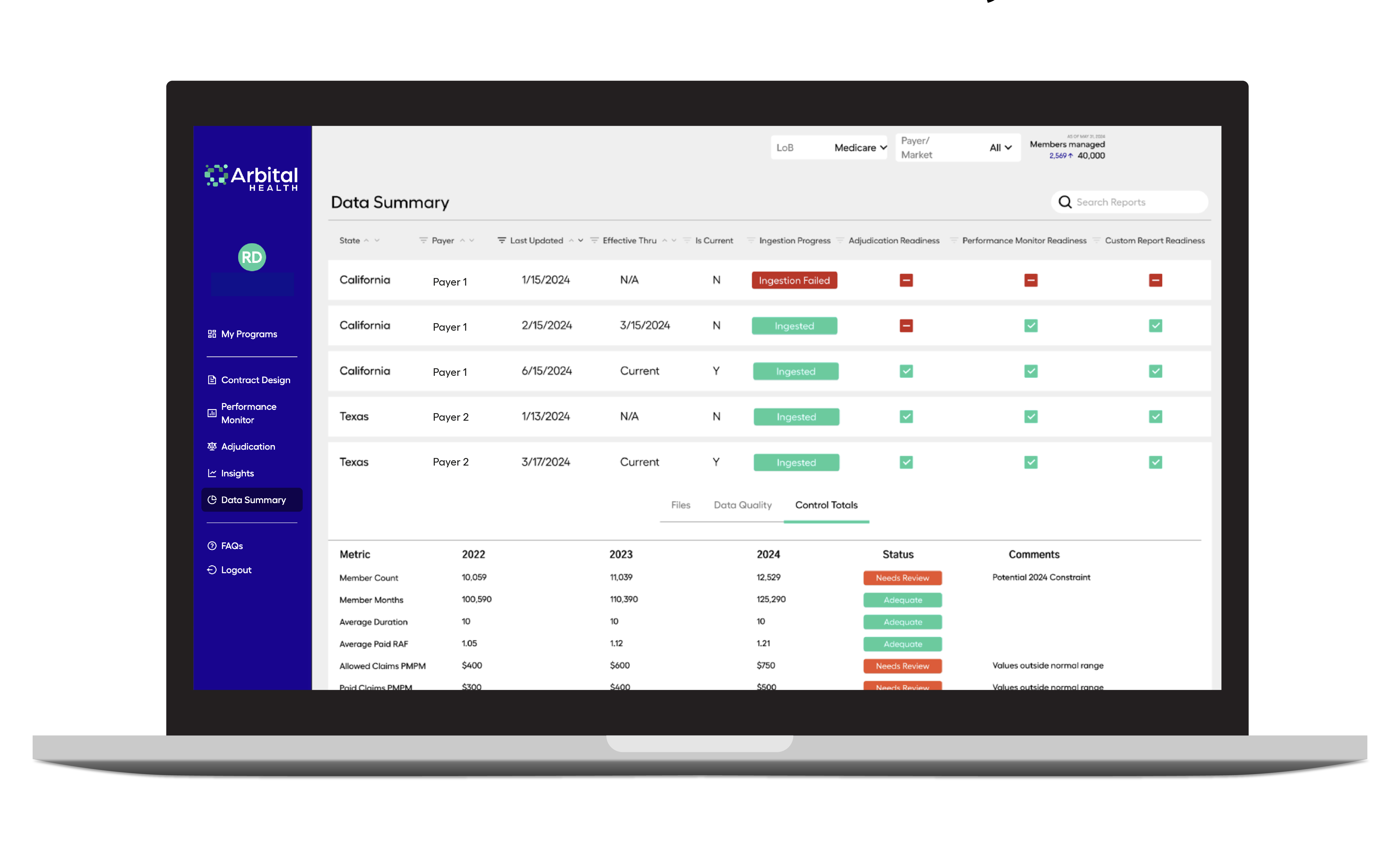
Data Ingestion & Enrichment
- Unlock trusted data quality and integrity assessment
- Validate your data with advanced actuarial calculations
- Analyze data against market-specific benchmarks
- Integrate seamlessly with various data file types
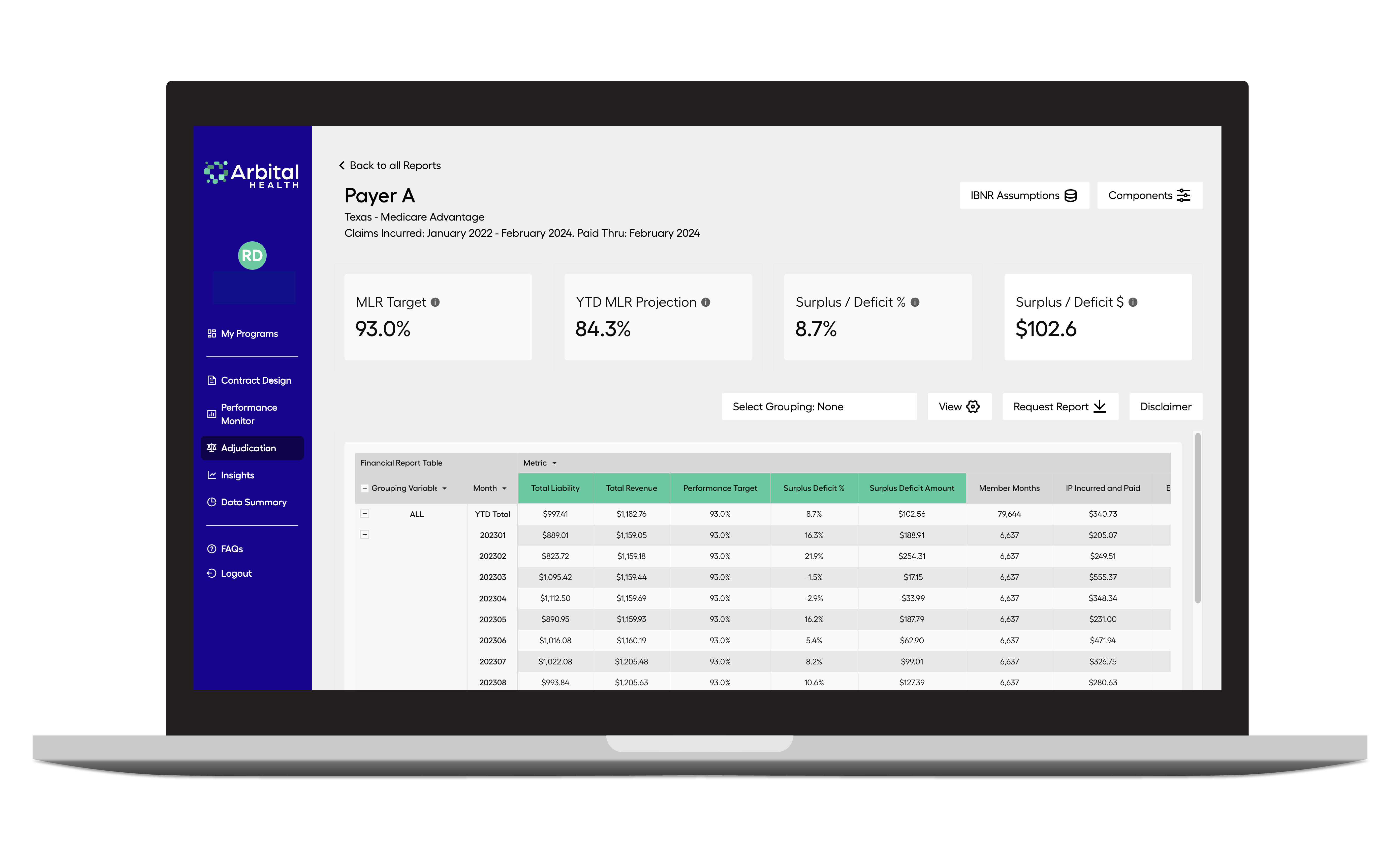
Adjudication Module
- Reconcile and forecast financial performance accurately
- Automate IBNR and MLR calculations
- Forecast surplus and deficit outcomes
- Ensure transparency and accountability among stakeholders
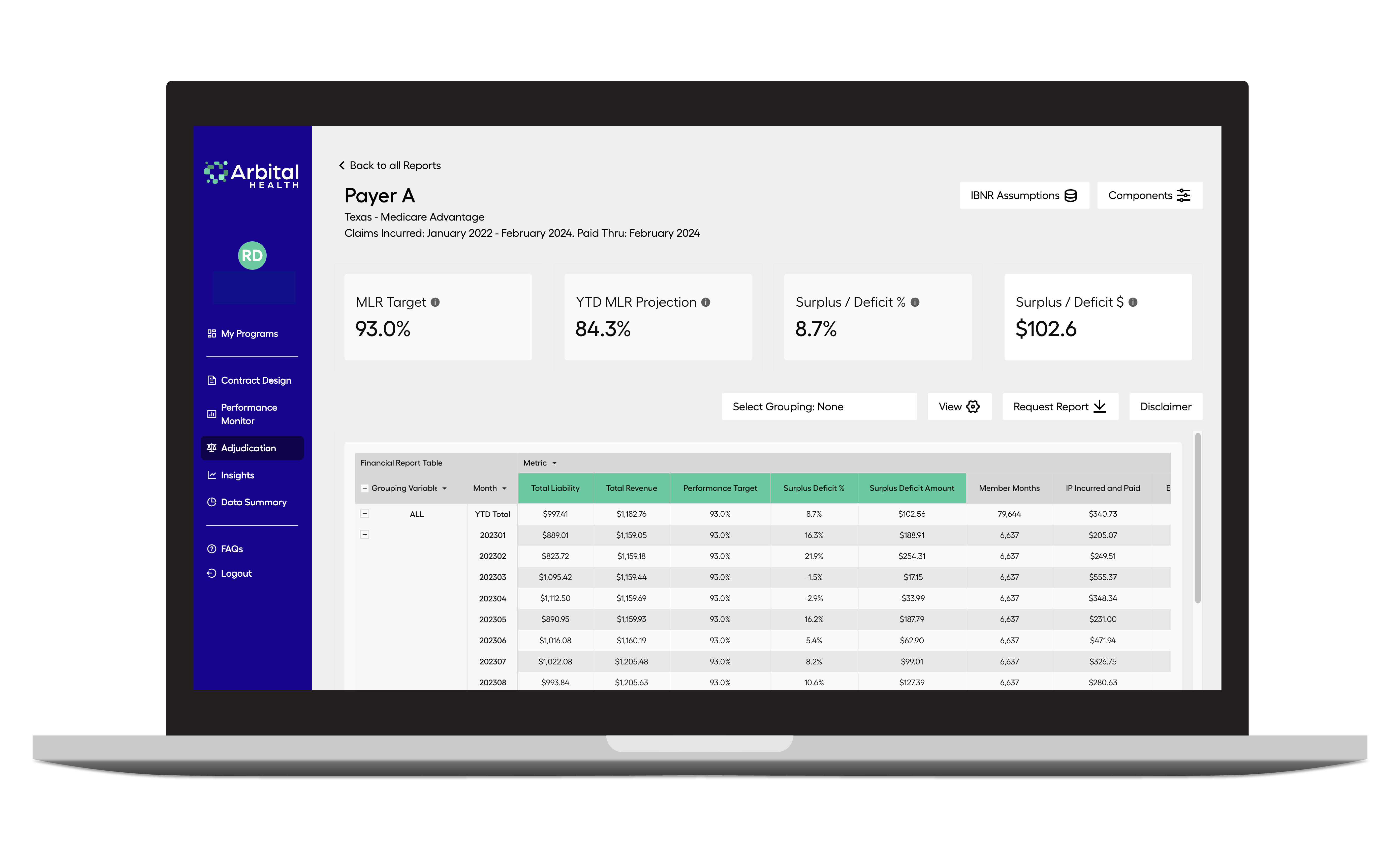
Adjudication Module
- Reconcile and forecast financial performance accurately
- Automate IBNR and MLR calculations
- Forecast surplus and deficit outcomes
- Ensure transparency and accountability among stakeholders
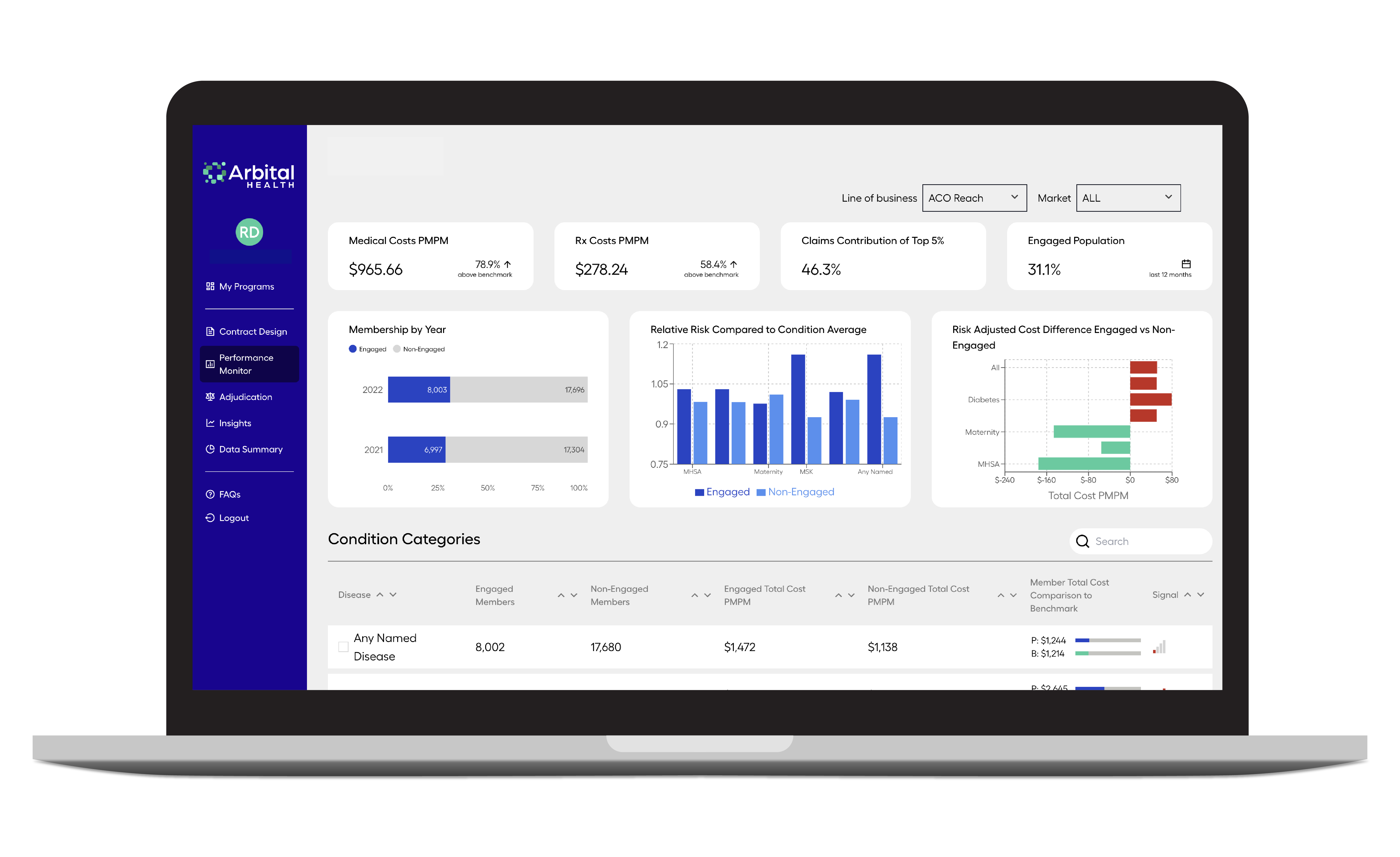
Performance Monitor Module
- Real-time contract performance monitoring
- Identify actionable opportunities to drive cost savings
- Compare your data to risk-matched benchmark populations
- Discover areas for improvement by identifying population health & operational needs
Insights Module
- Customize member data reports by health condition
- Segment data by line of business, payer, or other meaningful cohorts
- Dive into condition-specific cost and utilization insights
- Identify avoidable and actionable spend areas
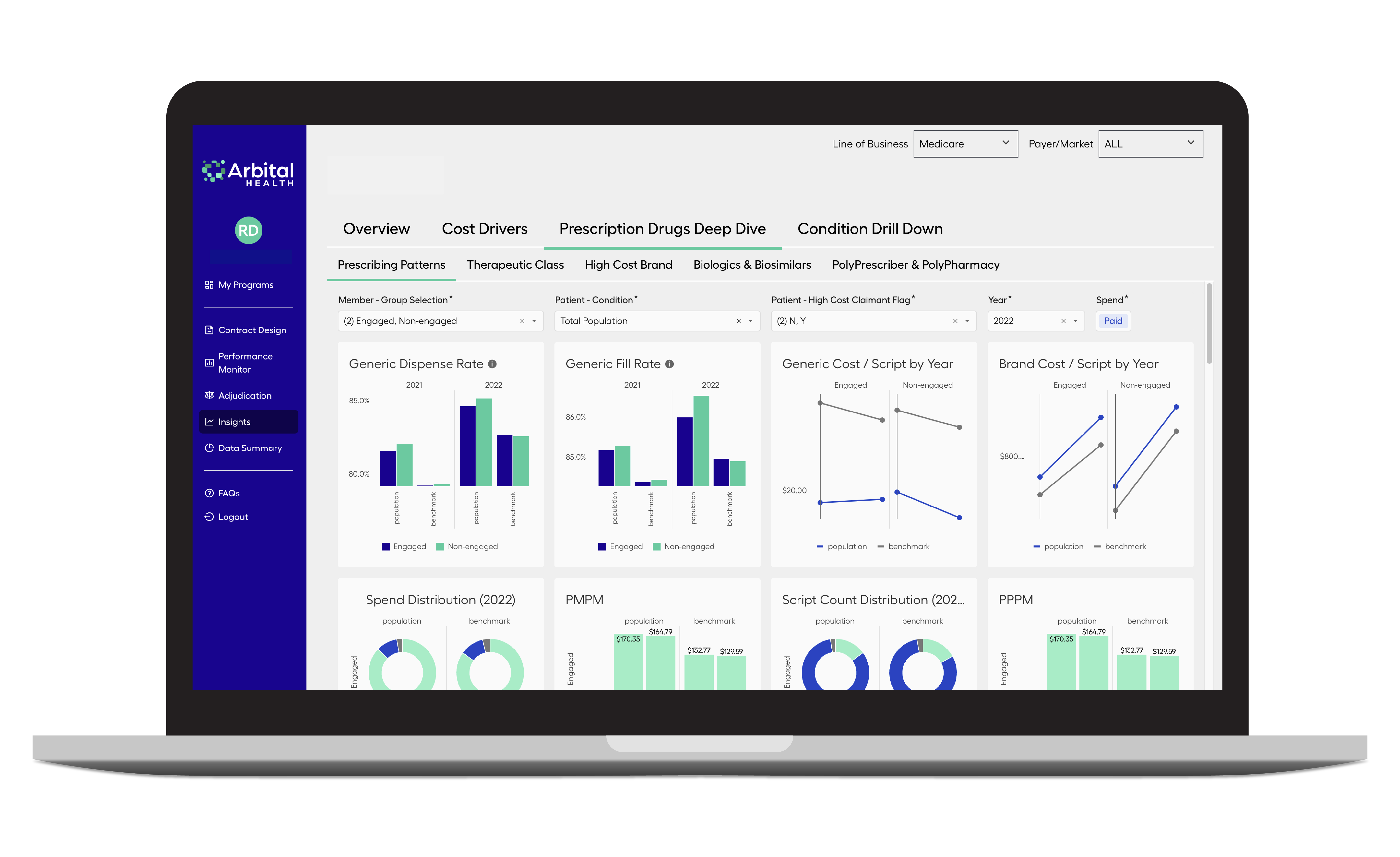
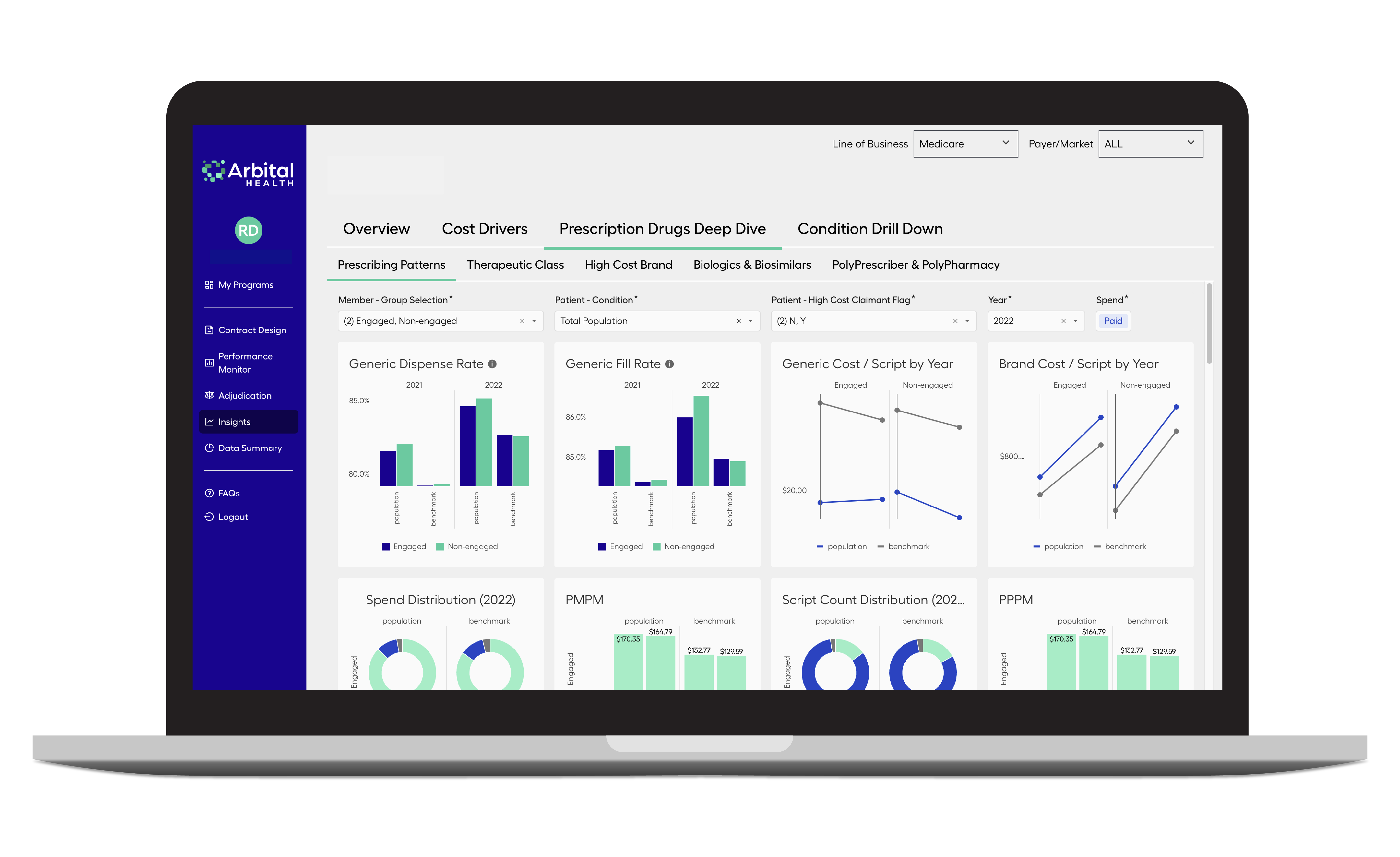
Insights Module
- Customize member data reports by health condition
- Segment data by line of business, payer, or other meaningful cohorts
- Dive into condition-specific cost and utilization insights
- Identify avoidable and actionable spend areas

